Health Assessment: Heart Disease in Doña Ana County
The following information is from the New Mexico Department of Health. View the full county health assessment.
Why Is This Important?
In 2017, heart disease was the leading cause of death in New Mexico and accounted for over 20% of all deaths.Risk and Resiliency Factors
Risk factors for heart disease include: high blood pressure, abnormal cholesterol, prediabetes, diabetes, tobacco use, secondhand smoke exposure, air pollution exposure, physical inactivity, poor nutrition, excessive alcohol consumption, and excess weight. Controlling and preventing these risk factors is crucial in reducing risk of developing heart disease as well as death from heart disease.How Are We Doing?
Generally, overall heart disease death rates have been decreasing for decades. However, heart disease and cancer deaths remain the top two leading causes of death in NM and the US.Age and Sex. As is common with chronic diseases, death rates increased as age increased, with a steep increase in the oldest age group (85+ years). In 2017, the heart disease death rate of males, 190.8 per 100,000, was statistically significantly higher than that of females, 116.1 per 100,000. This relationship to sex was seen across all but the youngest age group, 0 to 14 years of age.
Race/Ethnicity: Heart disease mortality varied greatly by race and ethnicity. During the 3-year period 2015-2017, in descending order from highest rate to lowest rate, each rate statistically significantly higher than all lower rates, the rates were: Black or African Americans, 213.3 per 100,000; whites, 154.2 per 100,000; Hispanic, 137.1 per 100,000; American Indian or Alaska Native, 121.5 per 100,000; and Asian or Pacific Islander (the lowest rate), 84.8 per 100,000.
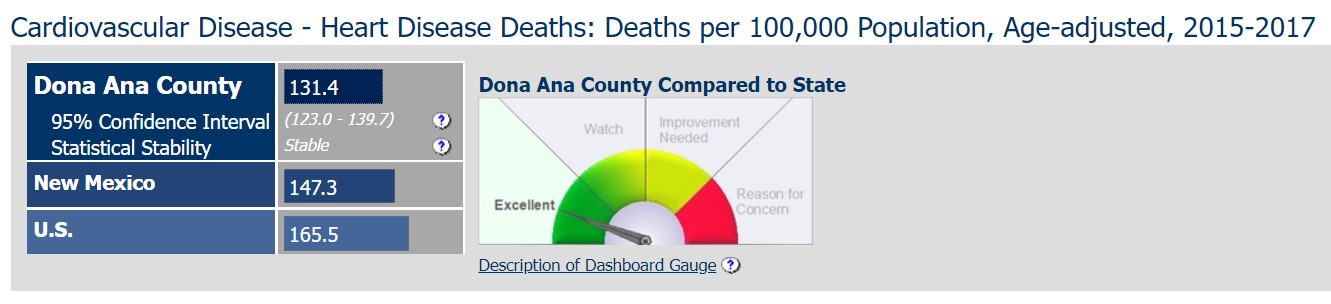
County: During the period 2015-2017, heart disease mortality rate varied by county. The six counties with the highest rates, five above 200 per 100,000, were Sierra, Chaves, Lea, Curry, Luna, and Eddy counties. The six counties with the lowest rates, all below 120 per 100,000, were Catron, Los Alamos, Santa Fe, Taos, Mora, and Harding.
Urban and Rural: NM counties were designated into four groups of urbanicity and rurality, using the National Center for Health Statistics classification scheme. For 2015-2017, heart disease mortality rates were highest and similar in Mixed Urban/Rural and Rural counties, and lowest in Metro and Small Metro counties. The heart disease mortality rate for Small Metro counties was statistically significantly lower than all other Urban/Rural categories.
What Is Being Done?
The NM Department of Health Heart Disease and Stroke Prevention (HDSP) Program within the Population and Community Health Bureau uses a comprehensive, evidence-based approach to promote healthy lifestyles focused on preventing, identifying and controlling high blood pressure and high cholesterol levels among New Mexican adults. Our mission is to improve the health of New Mexicans by implementing and evaluating effective strategies for cardiovascular disease prevention and management.The HDSP program and its partners work with communities, health systems, health care providers and other organizations across the state to implement activities that improve quality of care as it relates to blood pressure and cholesterol control. This will reduce CVD-related illness, save lives and be a valuable investment in population health.
Program strategies include:
- Assist health systems in tracking and monitoring clinical measures to improve health care quality and identify patients with high blood pressure
- Encourage team-based care practices within health systems
- Promote sustainability of community health workers/community health representatives/promotoras
- Increase the use of self-measured blood pressure monitoring with clinical support
- Facilitate referral of adults with high blood pressure or high blood cholesterol to community programs/resources
- Advance health equity to improve health outcomes and quality of life
- Increase the HDSP?s capacity to achieve and sustain program goals and strategies
The HDSP program consults with populations that are disproportionately affected by cardiovascular disease and stroke and/or those that serve them to develop education and services that are culturally appropriate to these populations.
Evidence-based Practices
Evidence-based community health improvement ideas and interventions may be found at the following sites:- The Guide to Community Preventive Services
- Health Indicators Warehouse
- County Health Rankings
- Healthy People 2020 Website
Heart Disease and its complications can be prevented and managed through these strategies:
- Clinical decision-support systems designed to assist healthcare providers in implementing clinical guidelines at the point of care.
- Reducing out-of-pocket costs (ROPC) for patients with high blood pressure and high cholesterol.
- Team-Based Care to Improve Blood Pressure Control.
- Interventions engaging community health workers/community health representatives/promotoras
- Implementing self-measured blood pressure monitoring interventions
- Interactive digital interventions for blood pressure self-management
- Mobile Health (mHealth) interventions for treatment adherence among newly diagnosed patients
CDC recommends specific major activities to implement these seven effective strategies:
- Implementation of CDSS at clinics and sites that provide healthcare services along with providing technical assistance on proper use of these systems.
- CDSS for cardiovascular disease prevention (CVD) include one or more of the following:
- Reminders for overdue CVD preventive services including screening for risk factors such as high blood pressure, diabetes, and high cholesterol
- Assessments of patients' risk for developing CVD based on their medical history, symptoms, and clinical test results
- Recommendations for evidence-based treatments to prevent CVD, including intensification of treatment
- Recommendations for health behavior changes to discuss with patients such as quitting smoking, increasing physical activity, and reducing excessive salt intake
- Alerts when indicators for CVD risk factors are not at goal
2) Reducing out-of-pocket costs (ROPC) for patients with high blood pressure and high cholesterol: - Reducing out-of-pocket costs involves program and policy changes that make cardiovascular disease preventive services more affordable. These services include:
- Medications
- Behavioral counseling (e.g. nutrition counseling)
- Behavioral support (e.g. community-based weight management programs, gym membership)
- Encouraging the delivery of preventive services in clinical and non-clinical settings (e.g. worksite, community).
- Promoting interventions that enhance patient-provider interaction such as team-based care, medication counseling, and patient education.
- Increasing awareness of covered services to providers and to patients with high blood pressure and high cholesterol using targeted messages.
- Work with diabetes management and tobacco cessation programs to coordinate coverage for blood pressure and cholesterol management.
3) Team-Based Care to Improve Blood Pressure Control: - Team-based care to improve blood pressure control is a health systems-level, organizational intervention that incorporates a multidisciplinary team to improve the quality of hypertension care for patients.
- Provide technical assistance to facilitate communication and coordination of care support among various team members including the patient, the patient?s primary care provider, nurses, pharmacists, dietitians, social workers, and community health workers.
- Enhance the use of evidence-based guidelines by team members.
- Actively engage patients and populations at risk in their own care by providing educational materials, medication adherence support, and tools and resources for self-management (including health behavior change).
4) Interventions engaging community health workers/community health representatives/promotoras: - Screening and health education. CHWs screen for high blood pressure, cholesterol, and behavioral risk factors recommended by the United States Preventive Services Task Force (USPSTF); deliver individual or group education on CVD risk factors; provide adherence support for medications; and offer self-management support for health behavior changes, such as increasing physical activity and smoking cessation.
- Outreach, enrollment, and information. CHWs reach out to individuals and families who are eligible for medical services, help them apply for these services, and provide proactive client follow-up and monitoring, such as appointment reminders and home visits.
- Team-based care. As care team members, CHWs partner with clients and licensed providers, such as physicians and nurses, to improve coordination of care and support for clients.
- Patient navigation. CHWs help individuals and families navigate complex medical service systems and processes to increase their access to care.
- Community organizers. CHWs facilitate self-directed change and community development by serving as liaisons between the community and healthcare systems.
5) Implementing self-measured blood pressure monitoring interventions: - One-on-one patient counseling on medications and health behavior changes (e.g., diet and exercise)
- Educational sessions on high blood pressure and blood pressure self-management
- Access to electronic or web-based tools (e.g., electronic requests for medication refills, text or email reminders to measure blood pressure or attend appointments, direct communications with healthcare providers via secure messaging)
6) Interactive digital interventions for blood pressure self-management: In these interventions, patients who have high blood pressure use digital devices to receive personalized, automated guidance on blood pressure self-management. Devices include mobile phones, web-based programs, or telephones. Interactive content does not require direct input from a health professional.
7) Mobile Health (mHealth) interventions for treatment adherence among newly diagnosed patients: mHealth interventions for treatment adherence use mobile devices to deliver self-management guidance to patients who have been recently diagnosed with cardiovascular disease. Content must be accessible through mobile-phones, smartphones, or other hand-held devices. Interventions must include one or more of the following: - Text-messages that provide information or encouragement for treatment adherence
- Text-message reminders for medications, appointments, or treatment goals
- Web-based content that can be viewed on mobile devices
- Applications (apps) developed or selected for the intervention with goal-setting, reminder functions, or both
- An interactive component (i.e., patients enter personal data or make choices) that gives patients personally relevant, tailored information and feedback
- Mobile communication or direct contact with a healthcare provider
- Web-based content to supplement text-message interventions
Healthy People Objective HDS-2:
Reduce coronary heart disease deathsU.S. Target: 103.4 deaths per 100,000 population
Relevant Population Characteristics:
- Death Rate from All Causes
- Death Rates from Leading Causes of Death
- New Mexico Population - Age 65+
- New Mexico Population - Education, No High School Diploma
- New Mexico Population - Median Household Income
- Years of Potential Life Lost (YPLL - Premature Mortality) Before Age 75
Risk Factors:
- Air Quality - Ozone Level
- Air Quality - Particulate Matter (PM2.5) Level
- Alcohol - Adult Binge Drinking
- Alcohol - Adult Heavy Drinking
- Cardiovascular Disease - Adult Ever Told Blood Pressure Was High
- Cardiovascular Disease - High Cholesterol
- Cardiovascular Disease - Prevalence
- Cardiovascular Disease - Stroke Deaths
- Diabetes (Diagnosed) Prevalence
- Obesity - Adult Prevalence
- Physical Activity - Adult Prevalence
- Tobacco Use - Adult Smoking Prevalence
Note
Some rows in data tables may include a note of Unstable or Very Unstable. Those rates labeled Unstable were statistically unstable (RSE >0.30 and <0.50), and may fluctuate widely across time periods due to random variation (chance). Those rates labeled Very Unstable were extremely unstable (RSE >0.50). These values should not be used to infer population risk. Data have been directly age-adjusted to the U.S. 2000 standard population.
Some rows in data tables may include a note of Unstable or Very Unstable. Those rates labeled Unstable were statistically unstable (RSE >0.30 and <0.50), and may fluctuate widely across time periods due to random variation (chance). Those rates labeled Very Unstable were extremely unstable (RSE >0.50). These values should not be used to infer population risk. Some Very Unstable rates have been suppressed.
Data Sources
New Mexico Death Data: Bureau of Vital Records and Health Statistics (BVRHS), New Mexico Department of Health. Population Estimates: University of New Mexico, Geospatial and Population Studies (GPS) Program, http://gps.unm.edu/. U.S. Data Source: Centers for Disease Control and Prevention, National Center for Health Statistics, ]http://www.cdc.gov/nchs/]Measure Description for Cardiovascular Disease - Heart Disease Deaths
Indicator Profile Report
Heart Disease Deaths per 100,000 Population (exits this report)
